New Report Helps Clinicians Improve Risk Stratification for Patients with Pulmonary Arterial Hypertension
Introduction
A new report is helping clinicians improve risk stratification for patients with pulmonary arterial hypertension (PAH) by providing consistency in grading systems of echocardiographic values. The report aimed to create consistency out of a number of observations about associations between echocardiographic values by analyzing them in the context of real-world patient outcomes. PAH is a life-threatening condition that affects the small arteries in the lungs, making it harder for the heart to pump blood through them. The report is published in the journal Pulmonary Circulation.
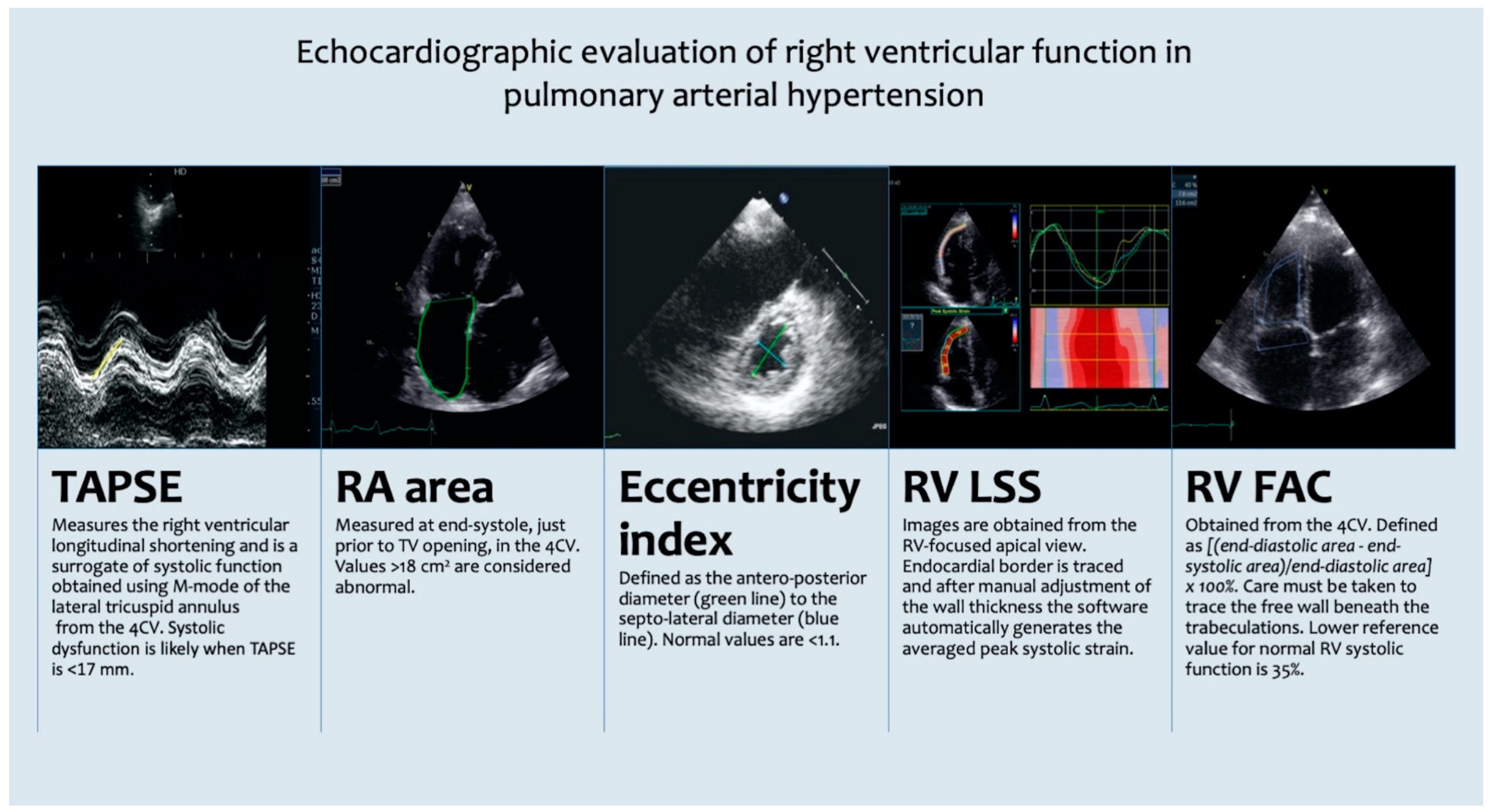
Mapping the Relationships between Right Heart Function Values
New research suggests that mapping out the relationships between right heart function values can help clinicians better risk-stratify patients with PAH. Corresponding author Bettia E. Celestin, PhD, of Stanford University, and colleagues, said a number of biomarkers for right heart failure have been identified in the past three decades. They noted that right heart failure is the most important cause of mortality in PAH. Those biomarkers include triscuspid annular plane systolic excursion (TAPSE), right ventricular (RV) free wall longitudinal strain, right ventricular end systolic dimension, and right atrial (RA) size and function.
Creating Consistency in Grading Systems
“With the multiplicity of right heart parameters, ensuring consistency in grading systems becomes even more important,” Celestin and colleagues said, writing in the journal Pulmonary Circulation. The team advises that one way to ensure consistency is to leverage the relationships between different right heart parameters. They noted, among other relationships, that a 2020 study found links between RV free wall longitudinal strain and right ventricular ejection fraction in patients with pulmonary hypertension. “These physiological relationships can help ensure consistency between thresholds for risk stratification,” they said. “In addition, they can help guide consistency between grading systems in PAH.”
Evaluating Relationships and Patient Outcomes
Celestin and colleagues set out to evaluate those relationships by comparing them to patient outcomes. They constructed a cohort of patients with Group 1 PAH who underwent right heart catheterization and echocardiography within 2 weeks of each other at Stanford Hospital. The patients were all adults, and their diagnoses came between 2002 and 2021. The authors evaluated a number of echocardiographic variables and then tracked patients to see which patients experienced death or lung transplant over the course of five years. At five years, 35% of patients had experienced either death or a lung transplant.
Echocardiographic Grading System for PAH
The authors then used those outcomes to create an echocardiographic grading system for PAH and used those thresholds to assess the Registry to Evaluate Early and Long-Term PAH Disease Management echocardiographic risk score (REVEAL-ECHO), which was published last year. In the latter analysis, they found REVEAL-ECHO scores were associated with survival in their validation cohort. The authors also found that REVEAL Lite scores correlated with patient outcomes. Those with a score of at least 8 had a 20% risk of death or transplantation at one year and a 50% risk at five years.
Implications for Clinical Practice
The investigators said the mathematical relationships they identified between right heart parameters have implications for clinical practice. For example, they said if a patient is found to have highly discordant RV fractional area change and RV free wall longitudinal strain values, further investigation is warranted to make sure the readings are accurate. “In addition, the strong association between many variables will likely simplify the number of features needed for phenomapping and profiling,” they wrote. “Finally, these mathematical relationships may further verify consistency in grading between metrics.”
Pulmonary Arterial Hypertension Treatments and Approvals
On the heels of Winrevair’s approval, Gossamer Bio and the Chiesi Group struck a deal to develop seralutinib. Winrevair is a newly approved therapy for PAH from Merck. Preliminary data suggest people with Group 1 PAH had improved outcomes if they had ever received hormone replacement therapy. Research shows health-related quality of life is impacted in major ways by PAH, but a solution to the problem—and the disease itself—has proven elusive.
New PAH Therapies and Approvals
This week, the FDA approved two therapies for PAH: Merck’s first in class therapy Winrevair and J&J’s oral combination tablet Opsynvi. The agency also approved Vafseo, a new treatment for anemia in kidney disease. The FDA granted full approval to the cancer drug Elahere and extended the indication of Vemlidy to children. Regulators also issued a CRL for odronextamab for lymphoma indications.
Sotatercept — now with the brand name Winrevair — will be available through specialty pharmacies by the end of April. The price of Winrevair is $14,000 per vial. J&J’s Opsynvi is single-tablet combination therapy containing macitentan which is an endothelin receptor antagonist and tadalafil that is a PDE5 inhibitor. It will be priced on parity with Opsumit, which is also a J&J product that treats patients with PAH.
Conclusion
In conclusion, the new report offers better consistency in grading systems of echocardiographic values for patients with PAH. The mathematical relationships identified between right heart parameters have implications for clinical practice as it will likely simplify the number of features needed for phenomapping and profiling. However, PAH remains a life-threatening condition, and research for better treatments and quality of life for patients with PAH are ongoing.
Originally Post From https://www.managedhealthcareexecutive.com/view/echocardiographic-grading-system-could-better-risk-stratify-people-with-pah
Read more about this topic at
variation and ‘drift’ by interpreter and practice site
Identifying consistent echocardiographic thresholds for risk …