Understanding the Tumor Microenvironment in Diffuse Large B-Cell Lymphoma (DLBCL)
Introduction
Diffuse large B-cell lymphoma (DLBCL) is a complex disease, both in terms of its genetic makeup and the role of the tumor microenvironment (TME) in its development and progression. Research into these aspects of DLBCL has shown great promise in terms of developing more personalized and effective treatments. In this article, we will discuss the latest findings in this field, with a focus on how evaluating the TME through immunohistochemical or molecular methods can lead to individualized and targeted treatments.
Heterogeneity in DLBCL
DLBCL is a heterogeneous disease, with different patients exhibiting varying degrees of TME composition and genetics. This heterogeneity has important prognostic and therapeutic implications, yet most cases, with the exception of primary nervous system tumors, are currently treated with the same regimens. By evaluating the TME and classifying tumors by cell of origin (COO), researchers hope to develop more individualized treatments that target different tumorigenesis pathways.
Cellular Markers and Genetics in the TME
Researchers have identified a number of cellular markers and genetics in the TME that play a significant role in tumor behavior and patients’ responses to treatment. These include endothelial cells, myofibroblasts, mast cells, lymphocytes, and macrophages. By understanding the biology of each component and its “crosstalk” with DLBCL tumor cells, researchers hope to develop more effective treatments.
Endothelial Cells
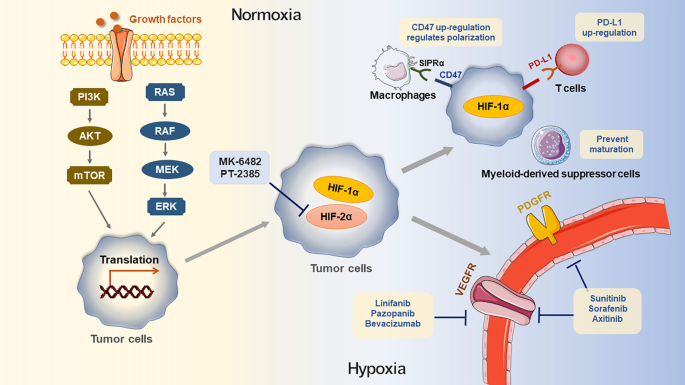
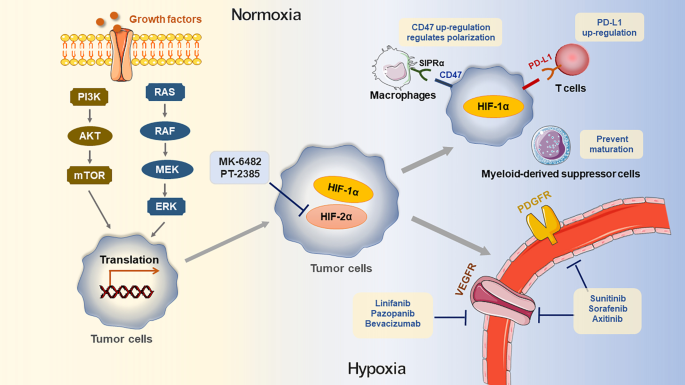
Endothelial cells play an important role in angiogenesis – the formation of new blood vessels. In DLBCL patients, tumor blood vessels differ significantly from normal vessels. However, follow-up of patients treated with anti-angiogenic agents such as anti–VEGF-A antibodies, bevacizumab, and R-CHOP has shown that increased vascularity in DLBCL patients may have only minor importance for the disease course.
Myofibroblasts
Myofibroblasts are stromal cells that play an integral role in lymphoma TME interactions. Overall, higher myofibroblast density is present in tumors that are associated with better outcomes. The results of one particular gene-expression profiling study showed that “the higher expression of myofibroblast, [dendritic cells], and CD4+ T-cell–related genes was correlated with better outcomes in DLBCL.”
Gene Expression Signatures in TME
The gene expression patterns of TME in DLBCL branch into a pair of distinct signatures, the stromal-1 signature, and the stromal-2 signature. The stromal-1 signature is marked by the TME’s high expression of extracellular matrix elements (i.e., osteonectin, collagen, laminin, fibronectin, thrombospondin, connective-tissue growth factor, remodeling proteins). The stromal-2 signature is highly vascularized, characterized by high expression of endothelial cell markers, VEGF receptor, endothelial tyrosine kinase, components of caveolae, and genes expressed in adipocytes, like RBP4 and ADIPOQ.
Conclusion
In summary, a deeper understanding and analysis of the TME in DLBCL can result in more individualized and effective treatments for patients. With the use of molecular and immunohistochemical methods, researchers can identify the cellular markers and genetics that play a significant role in tumor development and progression, leading to tailored treatment plans based on each patient’s unique situation.
Long-Tail Keywords: Tumor Microenvironment in DLBCL, Immunohistochemical Methods, Molecular Methods, Cellular Markers, Genetics, Myofibroblasts, Stromal-1 Signature, Stromal-2 Signature, Targeted Treatments.
Originally Post From https://www.ajmc.com/view/how-the-tumor-microenvironment-affects-dlbcl-prognosis-treatment
Read more about this topic at
Methods for assessment of the tumour microenvironment …
The tumor immune microenvironmental analysis … – Nature