Blood-Based Screening for Lung Cancer: A Game-Changer in Early Detection?
The world of healthcare keeps evolving, and one of the most exciting shifts in recent years has been the rise of blood-based screening tests for lung cancer. This approach is shaking up current screening methods and could offer a fresh way to spot lung cancer earlier than before. While the idea of using a simple blood sample might sound almost too good to be true, experts are cautiously optimistic about its potential to change early detection strategies, particularly for patients with a high risk but who are not currently part of low-dose CT screening programs.
For many, the road to lung cancer diagnosis is filled with tricky parts and tangled issues. Traditional methods like low-dose computed tomography (CT) scans can be intimidating, expensive, and sometimes miss early-stage cancer altogether. In contrast, the new blood-based tests could provide a more accessible and less nerve-racking alternative. This editorial takes a closer look at the promising results from recent studies, discusses the benefits and challenges of these screening tools, and examines what this could mean for patients and clinicians alike.
Advancements in Blood Screening for Early Lung Cancer Detection
Recent research findings have highlighted that blood-based tests might be capable of detecting lung cancers up to one year before traditional diagnostic methods would. In one notable study, the Mercy Halo blood-based lung screening test detected 31% of lung cancers a year before in-trial diagnosis compared with just 8% detected by low-dose CT scans interpreted with the Lung Imaging Reporting and Data System (Lung-RADS). Such a staggering difference in early detection rates suggests that blood-based testing could be a critical piece in the lung cancer screening puzzle.
One particularly appealing aspect of these tests is their potential to pick up on cancers that standard imaging might miss. Since the blood assay achieved a sensitivity nearly on par with low-dose CT (31% vs. around 40% in specific missed cases), it may serve as a useful complement that can flag cancers which would otherwise slip through the cracks. Given these advantages, experts are beginning to see blood-based screening as a must-have tool in the quest for earlier, more effective lung cancer detection.
Comparing Screening Modalities: Blood Tests Versus Low-Dose CT Scans
Low-dose CT scans have long been the cornerstone of lung cancer screening for high-risk individuals. However, they come with their own set of challenges and complicated pieces:
- Detection Rates: Traditional low-dose CT scans detect lung cancers in roughly 8% of patients within one year prior to diagnosis in standard frameworks. The blood-based approach, in contrast, picks up 31% of cases in a similar timeframe.
- Missed Diagnoses: In scenarios where low-dose CT scans using Lung-RADS miss some cancers, blood tests show promise by identifying nearly 40% of those cases.
- Sensitivity Over Time: Studies have observed that the sensitivity of CT screening decreases as the diagnostic window expands. For example, sensitivity can drop from around 86% at baseline to almost 58% after 36 months, revealing a series of twists and turns in measuring test performances over time.
A simplified table below helps illustrate the differences between these two methods:
| Screening Method | Detection Rate (1 year prior) | Sensitivity at Baseline | Sensitivity Over 36 Months |
|---|---|---|---|
| Low-Dose CT (using Lung-RADS) | 8% | ~86% (initial baseline) | ~58% (at 36 months) |
| Blood-Based Test (Mercy Halo) | 31% | N/A | Comparable to CT in overall sensitivity (~34-39%) |
This side-by-side comparison emphasizes not only the potentially life-saving benefits of earlier detection with blood tests but also the intricate trade-offs that come with each method. Ultimately, both tests have areas where they excel and areas where they confront their own set of challenging bits.
Improving Access for At-Risk Populations
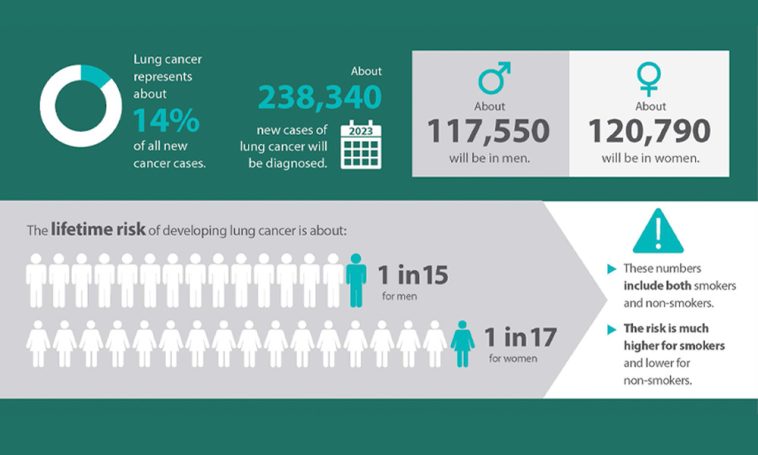
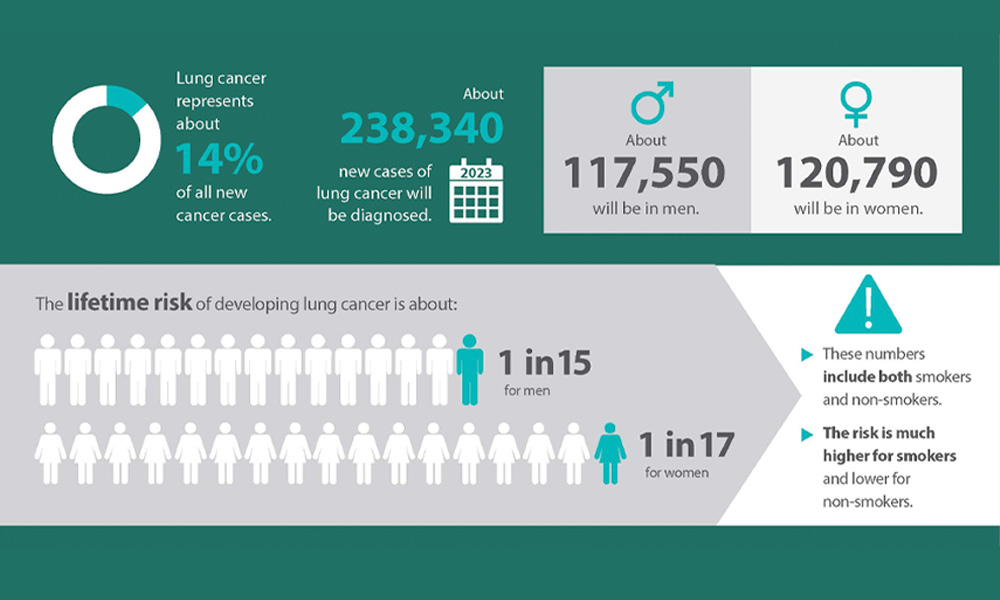
Lung cancer remains one of the leading causes of cancer-related death, with early detection being key to improving survival rates. According to the American Lung Association’s recent report, only 28.1% of lung cancers are caught at an early stage, when the 5-year survival rate is around 65%. This leaves a huge gap, as nearly half of the cases are diagnosed at a much later, more intimidating stage with survival rates dropping significantly to near or below 10%.
For patients at high risk who cannot or do not undergo regular CT scanning, a blood-based test presents a more accessible and less overwhelming alternative. The test’s ability to reliably identify preclinical disease means that clinicians could start treatment earlier, which is often directly linked to better outcomes. In practical terms, this tool might empower doctors to find your way through the maze of lung cancer detection sooner, thereby opening the door to timely interventions.
Benefits for Patients and Clinicians
The promise of blood-based lung cancer screening offers various advantages for both patients and healthcare professionals:
- Ease of Use: A blood test is generally less intimidating than a CT scan and can be performed quickly during a routine checkup.
- Improved Early Detection: With higher preclinical detection rates, patients have the opportunity for earlier treatment when the disease is less advanced.
- Enhanced Follow-Up: For patients who regularly undergo screenings, tracking changes in test scores over time (such as a 79% average increase in detected cases across successive rounds) can help tailor more personalized treatment plans.
- Complementary to CT Scans: Even when CT scans are available, the blood-based test can serve as an adjunct, identifying cases that might be overlooked by imaging alone.
Both clinicians and patients appreciate that with a blood-based screening tool, the diagnostic process may become less nerve-racking and more efficient in sorting out which patients need further evaluation and timely care.
Addressing the Tricky Parts: Challenges and Concerns
No diagnostic test is perfect, and with any new technology, there are some tricky parts and tangled issues that need careful consideration. One major concern is the balance between sensitivity (identifying true positive cases) and specificity (avoiding false positives). Although early studies have shown that blood-based tests approach the sensitivity of CT scans, ensuring that these tests do not result in too many unnecessary follow-up procedures is critical.
Another area full of problems is understanding how blood-based tests can be integrated into current screening protocols without overwhelming clinicians with extra data or complicating the decision-making process. The fine points include:
- Interpreting Test Scores: Averages, such as the 79% increase seen over sequential rounds, need to be clearly calibrated and understood so that clinicians can better gauge when a repeat test or intervention is necessary.
- Cost and Accessibility: As with any novel test, there will be concerns over cost, insurance coverage, and whether the test is available in rural or under-served areas.
- Standardization: Before widespread adoption, the test must be standardized across different laboratories and healthcare facilities to maintain consistent quality and reliability.
Critically, physicians and medical administrators must figure a path toward incorporating these new tests without adding undue hurdles. In practical terms, this means developing clear guidelines on who should be tested, how often, and what the follow-up steps should be if abnormal results are found. There is a need to address these tricky parts with relevant training and robust quality control measures.
Diving Deeper into the Data: Understanding Studies and Statistics
Recent studies, including those presented at reputable medical conferences, have offered a wealth of statistics that support the role of blood-based screening tests. For instance, the National Lung Screening Trial (NLST), which compared low-dose CT scans and chest x-rays, has provided a baseline against which the new test can be compared. Researchers found that even in a large cohort of over 53,000 patients, the sensitivity of imaging varied over time, underscoring the importance of a complementary test that could pick up cancers in earlier, preclinical stages.
One particularly fascinating statistic noted that while CT scan sensitivity at baseline was high (around 86.3%), it declined over time—dropping to nearly 58% at 36 months. This kind of data suggests that blood-based testing could help fill in the gaps where imaging technologies might struggle as time goes on. In practice, using both methods in tandem could lead to a more nuanced approach where the two tests cover each other’s blind spots.
Breaking down these statistics into digestible bullet points, we get:
- Blood-based test detection rate: 31% one year before clinical diagnosis.
- Low-dose CT scan detection: 8% within the same timeframe.
- Incremental improvement: The investigational test score increased by 79% over successive annual screenings.
- Complementary role: Blood tests identified 40% of cancers that CT scans missed using Lung-RADS.
By working through these numbers, it becomes clear that blood-based screening is not just a gimmick but a promising tool with the potential to reshape early lung cancer detection protocols. Having a better handle on these statistics can empower both clinicians and patients to make informed decisions about their health screenings.
Sorting Out the Future: What Lies Ahead for Lung Cancer Screening?
Looking forward, the integration of blood-based screening into routine lung cancer detection protocols is super important for several reasons. First, there is the issue of accessibility. Many high-risk patients are not part of a regular low-dose CT screening program due to various reasons—from living in rural areas to being deterred by the seemingly nerve-racking process of imaging studies. Incorporating a simple blood test could democratize early detection and give more Americans a chance at timely intervention.
Second, combining blood-based tests with imaging could lead to a more efficient, targeted screening process. By using both methods, physicians may be able to figure a path toward identifying patients who would most benefit from more detailed imaging or immediate treatment. This layered strategy could help mitigate the false positive and false negative rates that sometimes plague individual screening methods.
Moreover, as technology improves, we can expect the sensitivity and specificity of these tests to improve further. Innovations in molecular biology and artificial intelligence are already making it possible to dig into the nitty-gritty of blood biomarkers, while advanced algorithms can help in charting the subtle details of what a positive test result might mean for a patient’s future risk.
Some of these future prospects include:
- Refinement of Biomarkers: Ongoing research is likely to refine the panel of biomarkers used in these tests, making them even more accurate.
- Integration with AI: Machine learning models may soon be able to predict cancer progression with even greater accuracy, using data from both blood tests and imaging studies.
- Customized Screening Protocols: With more data, screening can become more personalized, adjusting the frequency and type of tests based on an individual’s unique risk profile.
- Cost Reduction: As these tests become more common, economies of scale may reduce costs, making it an even more attractive option for healthcare systems worldwide.
Though this road ahead is not without its twists and turns, the potential rewards are substantial. Future clinical trials and long-term studies will be essential in validating these approaches, but early results are promising enough to suggest that we are on the cusp of a major breakthrough in lung cancer screening.
Integrating New Technologies: Overcoming the Tangled Issues in Implementation
Introducing any new diagnostic tool into an already complex healthcare system is bound to be loaded with issues. One common concern is how to safely and effectively incorporate blood-based tests in tandem with existing screening protocols. Healthcare providers must figure a path through a range of regulatory, financial, and logistical challenges that are often full of problems.
Key areas to address include:
- Training and Education: Healthcare professionals need to be digitally literate about these tests—their advantages, limitations, and the interpretation of their results—to ensure that they can integrate them into standard care practices seamlessly.
- Regulatory Approval: As with any new test, obtaining and maintaining approval from regulatory bodies such as the FDA is a critical step that requires rigorous evidence and continuous monitoring.
- Reimbursement and Cost Issues: Insurance companies and healthcare payers must be convinced of the cost-effectiveness of blood-based screening, an effort that may require extensive data and pilot programs.
- Patient Acceptance: Finally, there is the task of educating patients about these new tests. Ensuring that patients understand the benefits—and the limitations—can help reduce anxiety and build trust in the process.
Ultimately, dealing with these tangled issues head-on will require collaboration among researchers, clinicians, policy makers, and patient advocacy groups. Stakeholder meetings, further clinical trials, and a transparent dialogue about both the good and the less satisfactory aspects of this emerging technology are all necessary steps in working through the challenges.
Opportunities to Enhance Personalized Medicine in Lung Cancer Care
One of the most promising aspects of the blood-based screening approach is the opportunity to push personalized medicine to the forefront of lung cancer care. Personalized medicine, which tailors treatment to an individual’s genetic makeup and disease profile, is becoming a key pillar in modern oncology. By identifying lung cancer at an earlier stage, blood tests not only promise to improve overall survival but also pave the way for more targeted treatment strategies.
In this context, the idea of “personalized screening” is especially compelling. With continued research, it’s possible that blood-based tests could eventually incorporate markers that are unique to a patient’s genetic predispositions or environmental exposures. This would allow doctors to design a screening program that is uniquely suited to each individual’s risk profile—a critical factor in the effective prevention and treatment of lung cancer.
Some benefits of this personalized approach include:
- Tailored Follow-Up: If a blood test detects early markers of lung cancer, follow-up imaging and diagnostics can be customized to the individual’s risk level.
- Optimized Treatment Planning: Early detection leads to more options when planning treatment, potentially shifting the focus to less aggressive methods that preserve quality of life.
- Reduced Uncertainty: For patients who may be on the fence about regular CT screening, a blood-based option presents a less intimidating way to keep tabs on their health.
- Cost-Effectiveness: Through better risk stratification, healthcare systems can allocate resources more efficiently, meaning that those who need intensive monitoring receive it promptly while minimizing unnecessary tests in low-risk populations.
This move toward personalized care in lung cancer is a clear illustration of how breakthrough technologies can transform disease management by fine-tuning the delicate balance between over-testing and under-detection.
Cornerstone Considerations for a New Screening Era
As we stand on the brink of a new era in lung cancer screening, there are several cornerstone considerations that must be kept in mind for the successful adoption of blood-based tests. These considerations involve not just the scientific and clinical facets but also the broader societal framework in which healthcare operates.
Some critical factors include:
- Evidence-Based Practice: Continued large-scale studies and long-term data will be vital in validating the effectiveness of these tests. Clinicians and researchers need rigorous evidence to overcome the inevitable skepticism that accompanies any new medical technology.
- Collaborative Research: To truly appreciate the subtle details of how blood-based tests perform in diverse populations, collaboration across institutions and even countries is essential. Pooling data will help refine testing protocols and ensure that the findings are broadly applicable.
- Technology Integration: Successful integration depends on building smart systems that can seamlessly combine data from blood tests, imaging, and clinical evaluations. This integration will help in making informed decisions without creating additional layers of complication.
- Patient-Centered Communication: It is super important for healthcare providers to communicate clearly with patients about the benefits as well as the limitations of new screening methods. Addressing any fears and helping patients understand the process will build trust and encourage participation in screening programs.
Each of these factors requires a balanced approach and careful planning, as any misstep could lead to confusing bits or even derail what might be a groundbreaking improvement in early lung cancer detection.
Conclusion: Paving the Way for a Healthier Future
In summary, the development of blood-based screening tests for lung cancer represents an exciting evolution in early detection strategies. By potentially identifying lung cancers at a stage when they are more treatable, these tests not only promise to enhance patient outcomes but also to reshape how we approach routine screenings for high-risk populations. The data so far indicate that these tests, if integrated with existing methods like low-dose CT scans, could help bridge the gap between early diagnosis and timely intervention.
However, as with any emerging technology, there remain several nerve-racking and tangled issues that the medical community must address. These range from ensuring high sensitivity and specificity to tackling regulatory, cost-related, and patient-acceptance challenges. Nevertheless, the initial results are promising, and the prospects of personalized and more accessible screening approaches are on the horizon.
As we look ahead, it is clear that the future of lung cancer screening will rely heavily on combined strategies. Healthcare providers, researchers, and policy makers must work closely together to figure a path through the practical barriers, ensuring that every patient stands a better chance at early and effective treatment. The opportunity to integrate blood-based tests with traditional imaging is both exciting and essential. It promises not only to improve diagnostic accuracy but also to empower patients in taking a more proactive role in their health care.
Moreover, embracing these innovative approaches can serve as a model for how the medical community can address other cancers and diseases. As technology continues to advance, it is incumbent upon us to dig into the subtle parts of new methodologies, refining the details and ensuring that every patient benefits from breakthroughs in modern medicine. While there is much left to be learned, the potential for a healthier, more informed future is within reach.
The journey ahead is certainly loaded with challenges, but it is also filled with exciting opportunities to revolutionize cancer care. For patients who have long waited for a less intimidating, more accessible screening option, the promise of a simple blood test is a beacon of hope. For clinicians, it offers another tool in the fight against a disease that has long been on edge with early detection difficulties. In this new era, the integration of blood-based screening could very well become the cornerstone of how we approach lung cancer—a shift that is critical for saving lives and improving overall quality of care.
By taking a step forward into this innovative territory, we not only honor decades of research and clinical practice but also set the stage for a future where early detection is less complicated and more reliable. In doing so, we pave the way for more personalized, targeted, and ultimately more effective cancer treatment strategies—a future where healthcare is centered around the needs of every individual, reducing uncertainties and fostering a better overall prognosis for those at risk.
In closing, while the road ahead might be riddled with tension and confusing bits, the potential benefits are enormous. It is through collaborative effort, continuous research, and a commitment to patient-centered care that we will be able to steer through these challenges. The advancements in blood-based lung cancer screening remind us that sometimes, the simplest solutions—a routine blood test—can have the most profound impact on saving lives.
As we continue to monitor emerging data and adjust our practices accordingly, there is every reason to believe that innovative screening methods will continue to evolve, offering hope and new possibilities to millions of Americans in the fight against lung cancer. The promise is here, and it is up to us to embrace it fully for a healthier future.
Originally Post From https://www.cancernetwork.com/view/blood-based-screening-test-may-increase-preclinical-lung-cancer-detection
Read more about this topic at
Exciting results from blood test for 50 cancers
FDA Clears First Blood Test Used in Diagnosing …