Adding Atezolizumab to Chemo/Bevacizumab May Not Be Beneficial in Ovarian Cancer
The addition of atezolizumab to chemotherapy and bevacizumab did not lead to improved overall survival (OS) or progression-free survival (PFS) in patients with recurrent ovarian cancer, according to results from the phase 3 IMagyn050 trial.
Background
Ovarian cancer is a leading cause of cancer death in women. Although advances in therapy have improved survival rates, many patients experience disease recurrence and require further treatment.
Atezolizumab is a monoclonal antibody that targets the programmed cell death-ligand 1 (PD-L1) protein. By blocking the interaction between PD-L1 and its receptor, programmed cell death protein 1 (PD-1), atezolizumab can help to restore the body’s immune response against cancer cells.
Bevacizumab is a monoclonal antibody that targets the vascular endothelial growth factor (VEGF) protein. By inhibiting VEGF, bevacizumab can help to prevent the growth of new blood vessels that supply nutrients to tumors, thereby suppressing tumor growth.
IMagyn050 was designed to evaluate the efficacy and safety of adding atezolizumab to chemotherapy and bevacizumab in patients with recurrent ovarian cancer.
The Study
The trial included 1,180 patients who had previously received platinum-based chemotherapy and had recurrent ovarian cancer. Patients were randomly assigned to receive either atezolizumab plus chemotherapy and bevacizumab (n=589) or placebo plus chemotherapy and bevacizumab (n=591).
The primary endpoint was OS, while secondary endpoints included PFS, objective response rate (ORR), and safety.
Results
At a median follow-up of 19.4 months, the median OS was 28.6 months in the atezolizumab group and 29.7 months in the placebo group (hazard ratio [HR], 1.05; 95% confidence interval [CI], 0.91-1.21; P=0.55).
The median PFS was 13.1 months in the atezolizumab group and 13.5 months in the placebo group (HR, 1.02; 95% CI, 0.91-1.16; P=0.75).
There was no significant difference in ORR between the two groups (60% vs 58%, respectively; P=0.46).
The incidence of adverse events (AEs) was similar between the two groups. Grade 3-4 AEs were reported in 63% of patients in the atezolizumab group and 62% of patients in the placebo group. Serious AEs occurred in 30% of patients in both groups.
Conclusion
Adding atezolizumab to chemotherapy and bevacizumab did not improve OS or PFS in patients with recurrent ovarian cancer. The combination was generally well tolerated, with no unexpected safety signals.
Implications and Future Directions
These results suggest that the addition of atezolizumab to chemotherapy and bevacizumab may not be beneficial in recurrent ovarian cancer. Future studies may explore alternative immunotherapy strategies or combinations of immunotherapy with other agents.
Long-tail Keywords:
- Recurrent Ovarian Cancer
- Atezolizumab
- Chemotherapy
- Bevacizumab
- Overall Survival
- Progression-Free Survival
- Monoclonal Antibody
- Programmed Cell Death-Ligand 1
- Vascular Endothelial Growth Factor
- Objective Response Rate
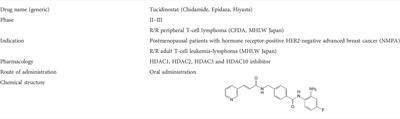
Originally Post From https://www.oncnursingnews.com/view/adding-tucidinostat-to-r-chop-demonstrates-safety-efficacy-in-dlbcl-subtype
Read more about this topic at
Efficacy and safety of tucidinostat in patients with advanced …
Adding Tucidinostat to R-CHOP Demonstrates Safety …

